AI in MedTech : AI-Powered Diagnostics and Predictive Care
Medical sensors, electronic health records (EHR), imaging systems, wearable devices, genomics platforms, and remote monitoring tools are producing unprecedented volumes of clinical and device-generated data every hour. Yet data on its own does nothing.
The core idea of AI in MedTech is simple: merge high-quality data with models, engineering, and workflow integration. This approach aims to create clear improvements in clinical outcomes. Value comes when raw signals turn into informed decisions. These lead to targeted interventions and smoother workflows. This makes care safer, more personal, & more efficient.
With the right healthcare AI solutions, underpinned by rigorous validation, explainability, and secure integration—organizations can close the loop from sensing to action: sense → analyze → decide → intervene → learn.
This article examines AI-driven healthcare innovation across data sources, and deployment roadmaps, with emphasis on AI integration in medical devices and AI-powered diagnostics to deliver AI for patient outcomes. Throughout, the focus remains constant: turning data into decisions that improve patient safety, quality, and experience.
AI Integration Feels Too Complex?
Fragmented data and complex workflows shouldn’t slow you down. We help MedTech companies turn data into accurate diagnostics and predictive insights.
Partner with us today!Understanding Healthcare Data: Sources, Challenges, and Promise
Sources of Data in MedTech
Data from an increasing number of sources are feeding medical devices and clinical systems:
- High-resolution imaging: High-resolution imaging provides clear views of the body. MRI, CT, and ultrasound scans show detailed anatomy.
- Physiological sensors: Continuous streams of ECG, SpO₂, blood pressure cuff & continuous glucose monitor (CGM) data, to name a few, provide a near real-time view of patient vitals.
- Wearables and implantable: Wearable devices such as smart insulin pumps and cardiac implants record long-term patient data from everyday life.
- Lab and genomic data: Biomarkers, ‘omics’ information (genomics, proteomics), and lab tests yield rich molecular-level information.
- EHR and clinical records: Both structured fields and unstructured clinician narratives hold a treasure trove of patient history and context.
- Remote patient monitoring: Home telemetry & mobile health apps take data collection outside the hospital.
- Device logs: Usage telemetry and maintenance records hold signals about device performance and potential faults.
Each stream is a river of potential insights about patient status, disease progression, and device performance.
The Challenges of Raw Data
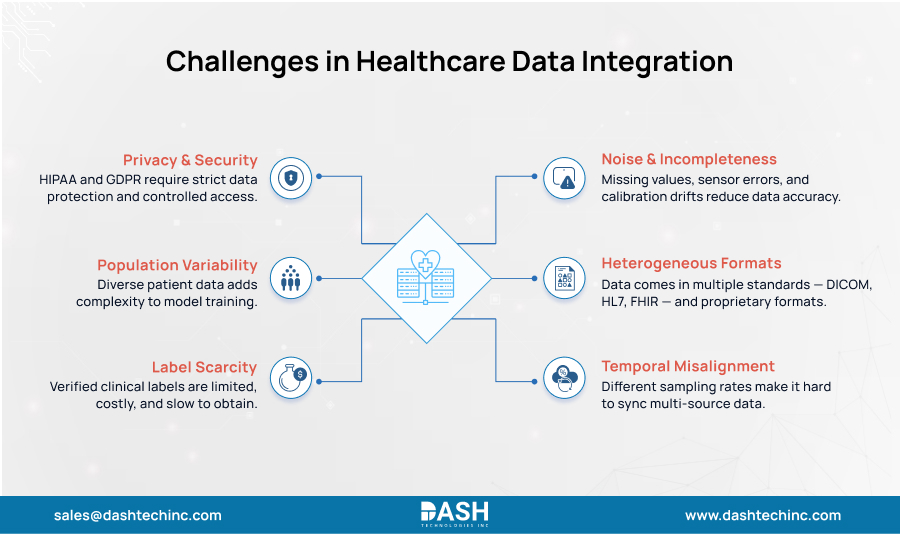
Real-world medical data is notoriously messy. It shows key friction points that stop organizations from using their data assets fully:
- Noise and incompleteness: It’s common to have missing values, sensor artifacts, & calibration drift.
- Heterogeneous formats: Data is in a mix of standards like DICOM, HL7, and FHIR, as well as a lot of proprietary device formats.
- Temporal misalignment: Integration of data from multiple sources at different sampling rates is a huge challenge in AI-driven healthcare innovation.
- Privacy and security: Access to and use of patient data are tightly controlled by regulations such as HIPAA and GDPR and require extensive security measures.
- Population variability: HIPAA and GDPR are two stringent laws that govern the use of patient data. These laws require strong security measures.
- Label scarcity: It is costly and time-consuming to get “ground truth” labels for training AI models. (E.g. a confirmed diagnosis, a definitive response to treatment.)
Why AI in MedTech (and Not Just Analytics) Is the Game Changer
Standard rule-based analytics and statistics are necessary, but AI and machine learning bring unique strengths to the table through healthcare AI solutions. They excel at:
- Capturing nonlinear, high-dimensional relationships that traditional methods lack.
- Learning from unstructured inputs like images, free-text notes, and complex waveforms.
- AI for patient outcomes detects subtle patterns, anomalies, and trends over extended periods of time.
- AI integration in medical devices enables predictive modeling, rather than just retrospective analysis.
In other words, AI in medical devices allows us to pivot from asking “what has happened” to “what may happen”—and most importantly, “what to do next.” This is the core of AI-driven healthcare innovation.
From Data to Better Outcomes — The Mechanism
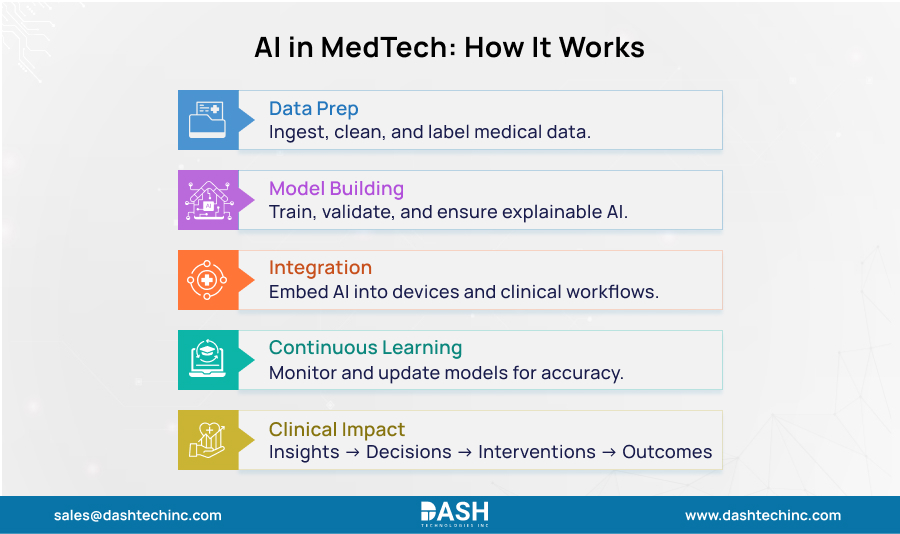
To appreciate how Healthcare AI solutions generate value, we need to dissect the data-to-outcomes pipeline into its essential components.
- Data Ingestion, Preprocessing & Labeling: The journey starts with solid pipelines that collect, sanitize, normalize, and synchronize streams of data. This is where high-quality data is labeled by experts to produce training sets. The absolute rule applies garbage in, garbage out.
- Model Training, Validation, and Explainability: The LLMs are trained and validated using strict protocols. This helps them perform well on new data and avoid overfitting. This process requires explainability modules, such as SHAP or LIME. These help clinicians see why a model made a certain recommendation. This helps build trust.
- Integration into Devices and Clinical Workflows: A great AI-driven healthcare innovation model is of no use if it isn’t integrated into the clinical workflow. This includes incorporating models into AI in medical devices, making it interoperable with EHRs, and designing efficient alerts and user interfaces. This is the essence of systems engineering for AI.
- Continuous Learning and Monitoring: Deployment is just the beginning. Models must be continuously monitored in the real world to detect performance drift. Retraining pipelines and version control are essential for maintaining the safety, calibration, & effectiveness of AI in the long term.
- Clinical Decision → Intervention → Outcome: The loop ultimately comes full circle. The AI provides insights to clinicians or automated systems. They then implement interventions and assess patient outcomes. This new data is being reintroduced into the pipeline. This creates a cycle of continuous improvement.
Barriers and Mitigations in Real Adoption
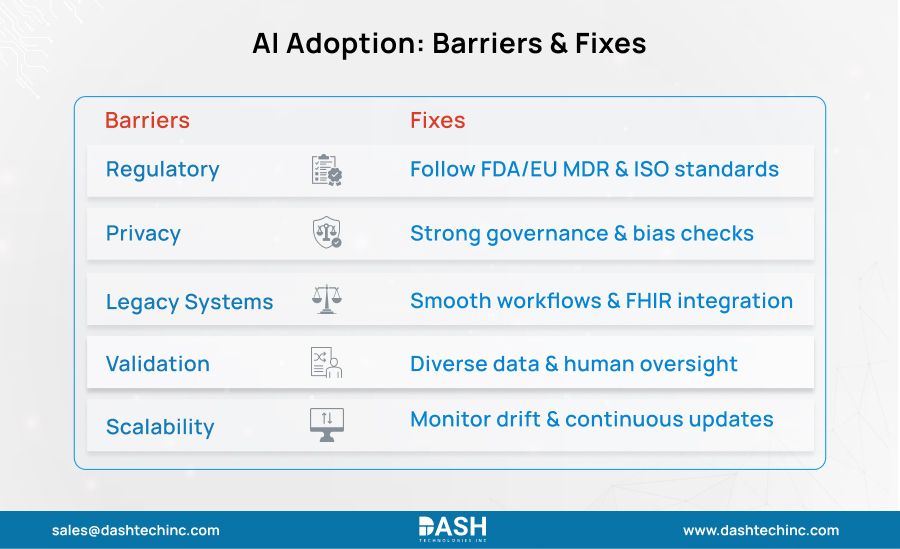
Regulatory, Safety, and Compliance
Frameworks from the FDA for AI/ML SaMD and IMDRF clinical evaluation require valid clinical association, analytical validation, and clinical validation, often within a total product lifecycle approach. The EU MDR Rule 11 moves most diagnostic and therapeutic decision-support software to higher classes. This increases evidence & post-market surveillance (PMS) requirements.
Mitigation: Align the IEC 62304 development process, ISO 14971 risk management, and ISO 13485 QMS in the early stages, and prepare (where applicable) for PCCP at the product development stage.
Data Access, Privacy, and Trust
The HIPAA Security Rule requires a risk analysis and safeguards for ePHI. Governance must cover de-identification, consent, and authorized use. WHO guidance emphasizes transparency, accountability, and equity to sustain trust as systems scale.
Mitigation: Employ strong governance, privacy‑enhancing techniques, and bias assessments with subgroup monitoring over time.
Integration with Legacy Systems & Workflows
Fragmented standards and old interfaces slow down adoption. Clinician trust depends on smooth, non-disruptive workflows. Interoperability via FHIR and modular APIs reduces friction and accelerates safe deployment.
Mitigation:
Work with clinicians to design solutions.
Simulate workflows.
Measure usability and safety during integration.
Validation in diverse populations
Reviews highlight a lack of strong evidence and little external validation. This raises concerns about performance gaps among different demographics and settings. Ethical guidance calls for inclusiveness and ongoing equity checks to prevent harm.
Mitigation: Use diverse datasets, perform external/temporal validation, and implement monitored fallback or human override.
Scalability and Maintenance
Models degrade with drift, hardware change, and new cohorts, necessitating disciplined updates and surveillance. Sustained impact depends on lifecycle MLOps and post‑market governance.
Conclusion
The path from raw health data to improved patient outcomes is challenging but possible. AI in MedTech helps us transform sensor signals, images, and clinical records. This leads to life-saving strategies for detection, prediction, and intervention. Success needs more than an algorithm. It requires a complete approach that includes data pipelines, explainability, integration, and governance.
To bring this vision to life, you need a partner who understands both medical devices & AI. If you’re a leader or innovator ready to drive AI healthcare forward, contact us. Let us help you turn your data assets into real patient impact.
About Dash

Dash Technologies Inc.
We’re technology experts with a passion for bringing concepts to life. By leveraging a unique, consultative process and an agile development approach, we translate business challenges into technology solutions Get in touch.







