Interoperability Challenges in EHR and EMR Software Solutions – And How to Solve Them
EHR and EMR software solutions are central to how healthcare organizations manage, access, and share patient data. As digital systems grow more complex, interoperability becomes a cornerstone for delivering safe and coordinated care. Without interoperability, even advanced systems may fail to provide meaningful outcomes.
In this blog, we’ll explore the main challenges that limit EHR and EMR system interoperability. You’ll also discover technology-driven solutions that improve data exchange and clinical outcomes.
What Is Interoperability in EMR and EHR?
Interoperability in EHR enables different healthcare systems to share and use patient data with minimal effort. It uses standards such as HL7 and FHIR to keep the information accurate and consistent. This helps doctors access the right records no matter where they treat a patient. It helps avoid duplicate tests and allows for faster decision-making during patient care. For it to work well, systems need structured data, secure APIs, and must follow privacy rules.
In contrast, EMR systems share patient information within one healthcare organization. EMRs help practices and departments record patient visits. But, when different departments use different systems, sharing structured data becomes essential. Structural and foundational interoperability lets EMR systems share data using a standard method, reducing duplication and improving internal processes.
Effective EHR and EMR software solutions allow for easy, safe, and useful sharing of information in any care environment.
Core Challenges Limiting Data Exchange in EHR/EMR Systems
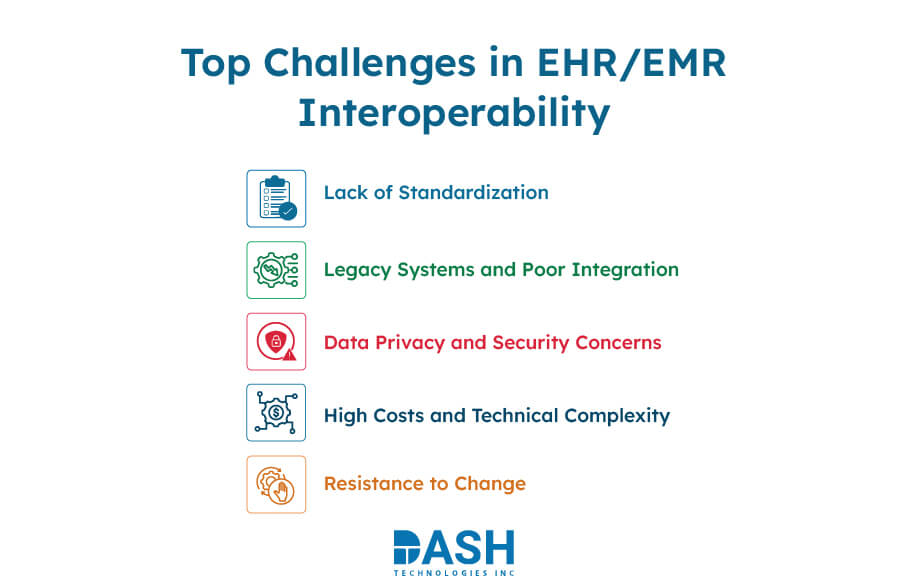
Achieving true interoperability in EHR and EMR systems goes beyond connecting platforms. It needs to tackle many technical, operational, and organizational barriers. These barriers disrupt smooth data exchange.
-
Lack of Standardization
Different vendors use varied data formats such as CDA (Clinical Document Architecture), JSON, or XML and communication protocols such as HL7 v2, HL7 v3, and FHIR, making interoperability difficult.
Without standardized frameworks, EHR/EMR systems can’t share and understand data effectively. This causes fragmented patient information and inconsistent data management, impacting care coordination and clinical decision-making. -
Legacy Systems and Poor Integration
Many healthcare facilities still use outdated systems. These old EHR systems usually aren’t compatible with modern tools and technologies. This leads to isolated systems, disrupting the exchange of patient information. Integrating newer systems and solutions require significant resources, and delays in upgrades slow down clinical and operational progress.
-
Data Privacy and Security Concerns
Secure and compliant transfer of private patient data between systems is critical. An EMR system must have encryption, access controls, and audit trails to protect patient data and monitor how it’s being used. It enables us to store data securely as well as stay compliant; while making sure it meets HIPAA standards. If such defenses vary from one system to another, there is enhanced risk of data breaches on both the providers and patients.
-
High Costs and Technical Complexity
Building and maintaining interoperability between EHR/EMR systems involves a significant investment. This includes expenses for software, integration tools, infrastructure improvements, and hiring or training technical staff. Smaller providers might find it hard to use interoperable EMR solutions. This can stress their finances and operations, especially with few IT resources.
-
Resistance to Change
Switching to modern EHR solutions often faces internal resistance in healthcare organizations. We need to retrain the staff, and we must adjust daily workflows to fit the new system. These changes can cause temporary disruptions, such as downtime and reduced productivity.
Real-World Impact of Poor Interoperability
Here are key areas where poor data exchange creates challenges for both providers and patients:
- Missed Patient Data
Without system-level interoperability, different facilities can scatter patient records. For example, if a cardiologist’s EMR lacks recent lab results from another hospital’s EHR, the doctor might miss important details. This can result in unnecessary tests, slower treatment, or decisions based on incomplete information. It also affects the continuity of care during post-hospital discharge follow-ups. Even small data gaps can disrupt care continuity and increase patient risk.Looking To Improve Your EHR/EMR Data Exchange?
Explore how you can simplify data sharing, reduce errors, and support better care—whether you're upgrading legacy systems or building new integrations.
View Our EHR/EMR Integration Services - Increased Administrative Burden
When systems aren’t integrated, front-line workers spend more time collecting patient information. They tend to use paper records, faxed reports, or even insecure emails to exchange data.
Various systems use different formats like XML, JSON, CSV, and PDF. This leads to confusion and delays in clinical workflows. More people are doing manual data entry now, so the chances of errors are going up. Most older systems do not support standards like FHIR or HL7. - Care Delays and Errors
Timely decisions rely on accurate information. In emergencies, allergy details, medication lists, and past treatment histories are crucial. If this information is hard to find, doctors may make mistakes. This can delay treatment and lead to medication errors or unnecessary treatments.
Using standards-based EHR and EMR software facilitates smooth data flow and minimizes clinical risk. Using integrated EHR solutions and EMR solutions reduces duplicate tests, leading to quicker care decisions at the point of care.
Solving Interoperability Challenges in EHR/EMR Systems
Healthcare providers must find practical ways to ensure secure and easy data sharing across systems. This will help tackle interoperability challenges with strong solutions.
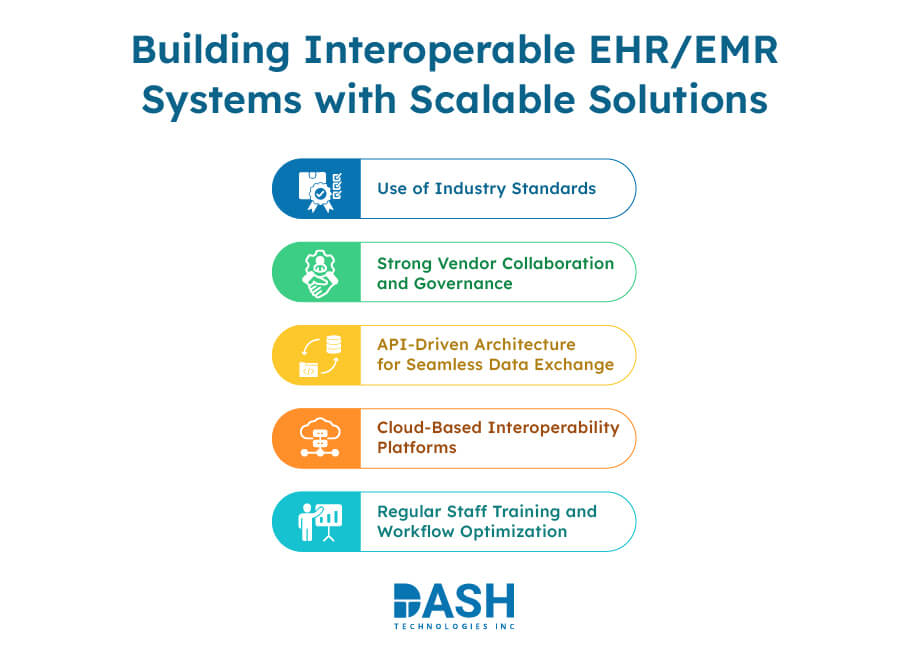
a. Use of Industry Standards
Using standards like HL7 and FHIR helps data move between systems. This keeps the context intact. These protocols ensure that data are consistent and understandable across all platforms. They make sure clinical terms, lab values, and imaging results are clear and helpful on every platform. FHIR supports modular data access through RESTful APIs, allowing real-time interoperability. Adopting these standards is foundational for scalable EHR and EMR software solutions in healthcare networks.
b. API-Driven Architecture for Seamless Data Exchange
Modern interoperability uses APIs for secure, real-time communication between systems. An API-first architecture keeps front-end apps apart from back-end data sources. This setup makes integration easier and reduces downtime during updates. Developers often use OAuth 2.0 and JSON Web Tokens (JWT) to manage secure API access. This approach supports EHR and EMR software that can adapt to new tech standards.
c. Cloud-Based Interoperability Platforms
Cloud infrastructure supports scalable data sharing across many organizations and care settings. Centralized data hubs allow healthcare providers to access records with convenience. This means that there is no need for any local storage. As a result, uptime improves, and infrastructure maintenance goes down. These platforms also support advanced analytics, enabling predictive insights from unified datasets. Cloud-native models play a key role in accelerating healthcare digital transformation across regions.
d. Strong Vendor Collaboration and Governance
Effective interoperability requires clear agreements among vendors on data format, sharing, and security. Governance models should define roles, data ownership, and accountability for clinical data exchanges. In multi-vendor environments, shared APIs, sandbox environments, and clear roadmaps are beneficial.
e. Regular Staff Training and Workflow Optimization
Interoperability tools are only effective when used properly by staff. Training helps clinical and administrative teams use data efficiently. They learn to access, interpret, and apply information to reach their goals. Workflow optimization aligns daily operations with system capabilities, reducing manual effort. Getting staff involved is key to making sure EHR and EMR software truly supports better patient care.
Conclusion
Interoperability is key for patient care, efficient operations, and meeting regulations. Challenges like standardization, legacy systems, security, and costs exist. But they can be overcome. Healthcare providers can improve system integration by using APIs, cloud services, industry standards, and providing staff training.
True data exchange begins with understanding the current EHR and EMR software solutions and spotting areas for improvement. Through focused effort, clear governance, and the right technology partners, interoperability can be achieved.
DASH offers tailored EHR/EMR integration solutions built around your workflows. Let’s connect to discuss your requirements!
About Dash

Dash Technologies Inc.
We’re technology experts with a passion for bringing concepts to life. By leveraging a unique, consultative process and an agile development approach, we translate business challenges into technology solutions Get in touch.